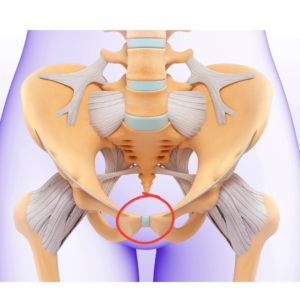
What is Pubic Symphysis Pain?
The pubic symphysis is a joint located at the front of the pelvis, where the left and right pubic bones meet. Pain at this location is sometimes referred to as symphysis pubic dysfunction (SPD) or pelvic girdle pain (PGP). PGP is a more general term general and can refer to pain that occurs in various areas throughout the pelvis, while SPD is more specific to the pubic symphysis region. SPD can result in difficulty with walking due to pain. Walking up and down stairs, on uneven terrain or even standing for long periods of time can be problematic. Some people will even express pain with getting in and out of bed, getting in and out of a chair, and raising one leg for any activity. Given how SPD can impact the ability to perform routine activities, it is important that we talk about various causes. We will also address conservative and non-pharmacological treatment options.
Understanding how the following situations and/or diagnoses can contribute to SPD is important and we will discuss each in more detail below.
- Pregnancy
- Osteoarthritis
- Infection
- Injury or direct trauma
Pregnancy and SPD
- Hormonal Changes: Relaxin and progesterone increase during pregnancy, loosening the ligaments in the pelvis to prepare for childbirth. Both of these hormones can contribute to increased laxity of ligaments and joints.
- Weight Gain: The additional weight of the growing baby puts extra pressure on the pelvic region.The uterus, placenta, and amniotic sac are all structures that place additional weight on the pelvic region. The pelvic floor muscles help to support the mentioned structures while continuing to support the bladder and rectum. However, the bones and ligaments in this region can still be impacted resulting in pain in the pelvis and specifically at the pubic symphysis.
- Postural Changes: As the pregnancy progresses, the body’s center of gravity shifts, altering posture and increasing strain on the pelvis. Most commonly the postural change that is seen is that the pelvis will begin to anteriorly tilt and lumbar lordosis increases. (As the baby grows the arch in the lower back appears to increase simply because of additional weight shifting the postural alignment.) These are not the only postural based changes that occur and can contribute to pubic symphysis pain. Changes in the feet and hips are possible and can impact postural alignment, and influence how well certain muscles activate.
Arthritis and SPD
The pubic symphysis region is a joint with a disc that is covered in fibrous tissue. This joint does not have large amounts of movement, but does allow for some mobility and shock absorption. Osteoarthritis is when joints begin to show signs of degeneration. Generally speaking, arthritis itself is not a disease process and we should expect some changes in joint surfaces as we age. However, there are certain things that can exacerbate osteoarthritis and result in increased joint pain. These can include genetics, infection, previous injury, chronic diseases, comorbidities, and lifestyle.
Infection at the Pubic Symphysis
Osteomyelitis can occur in this region and is an infection involving the bone. This is extremely rare at this location and can have debilitating symptoms due to the pain associated. This is generally diagnosed with imaging, lab work, and potentially a biopsy. Osteomyelitis requires antibiotics for treatment and in some cases may need surgical debridement as well.
Previous Pelvic Injury
A history of pelvic trauma and/or injury can increase the risk of developing SPD. Trauma to this area can result in pain. For some individuals this pain may be brief and only last for a short period of time, and for others it may result in long-term symptoms. The type and degree of injury can contribute to the potential risk for long-term pain. One form of diagnosis that is the direct result of trauma that can occur in this area is pubic symphysis diastasis. This is when the pubic bones are separated, and this form of diastasis is very rare.
Managing Pubic Symphysis Pain
While pubic symphysis pain can be challenging, several strategies can help manage and alleviate symptoms. Here are some strategies that a physical therapist can assist with to help manage and treat the pain. You will also find recommendations for products that I have used with my own patients.
1. Pelvic Support Belts: Wearing a pelvic support belt can help stabilize the pelvis and reduce pain. Oftentimes these belts are referred to as sacro-iliac (SI) belts and add compression to the pelvic region to help minimize the occurrence of pain at the pubic by decreasing shearing forces.
Check out this video to learn how to use an SI Belt.
*One of the most important factors that is often not considered when getting an SI belt is to make sure you get the correct size. Be sure to look at the sizing chart for the various brands so that you order the correct size. Here are a few options that I recommend.
2. Transcutaneous electrical stimulation (TENS): Using a TENS unit with pads placed over the low back region can help to address pain at the pubic symphysis. This is a non-invasive treatment that your physical therapist can teach you to use independently and for use throughout the day as needed.
*A TENS unit that I generally recommend is the TENS 7000. This machine is not pre-set and a physical therapist can help you set it up appropriately. I prefer this over preset machines because you have the ability to better customize and it tends to have a stronger output if needed. Please follow the recommendations of the manufacturer when using.
3. Exercise: Performing exercises to help strengthen the hips and core can be helpful in allowing for muscles to help provide additional stability and minimize the shearing that can occur at the pubic symphysis. Starting with exercises such as squeezing a ball or towel between the knees and pushing the knees out into a belt can be helpful. It can also be helpful to do activities to help strengthen your gluteal muscles such as bridges. These exercises are generally lower intensity and can be performed with the pain well managed. As this improves, progressing to more challenging activities such as modified lunges and side-stepping can continue to help with progression towards tolerating more functional based movements common to everyday life.
Here is a video of some exercises to consider. For all of the exercises make sure you do not push into heightened levels of pain. Also, the standing exercises are not always appropriate earlier on and many will need to work up to these.
6. Hands-on treatment: Providing hands-on, manual, treatment that targets the pubic symphysis and surrounding joints can be helpful with managing pain. Using techniques to address painful and sore muscles can help to improve motion and decrease restrictions. Some physical therapists are able to perform techniques such as dry needling to help manage pain when appropriate.
5. Warm or cold therapy: Applying warmth to the affected area can help soothe pain and reduce muscle tension. Warmth can also help to increase the circulation to an area. This can be accomplished by using a heating pad as needed over the painful region. Cold therapy can also be helpful for some, especially if there is a lot of inflammation. Using an ice pack over the painful area can help to decrease pain and also decrease inflammation.
*Here are some suggestions on cold and hot packs. Using a cold pack that is gel-based can help to better mold to your body. For both a cold and hot pack I recommend using a barrier between it and your skin. Be sure to check your skin before and afterwards. For both cold and hot packs, if it feels too cold or too hot please remove. Also, do not fall asleep with these in place. Please follow the recommendations of the manufacturer when using.
When should you seek help?
The answer is simple. As soon as you notice the symptoms and recognize that it is impacting your normal routine, you should seek help. Seeing a physical therapist can help you address the pain. A physical therapist can also determine if your presentation would warrant a referral to another medical provider for further examination and testing. In some states within the United States and also countries throughout the world, physical therapists are able to order imaging. A physical therapist can assist you with determining the cause of SPD and also effectively provide treatment.
A few references for you. Enjoy!
Howell ER. Pregnancy-related symphysis pubis dysfunction management and postpartum rehabilitation: two case reports. J Can Chiropr Assoc. 2012 Jun;56(2):102-11. PMID: 22675223; PMCID: PMC3364059.
Yax J, Cheng D. Osteomyelitis pubis: a rare and elusive diagnosis. West J Emerg Med. 2014 Nov;15(7):880-2. doi: 10.5811/westjem.2014.8.13401. Epub 2014 Oct 7. PMID: 25493141; PMCID: PMC4251242.
*As an amazon affiliate, I may be eligible for commission on certain products.
whoah this blog is magnificent i love reading your posts. Keep up the great work! You know, a lot of people are looking around for this info, you can help them greatly.